Foot Drop After Stroke: Is the Problem in Plantar Flexors or Dorsiflexors?
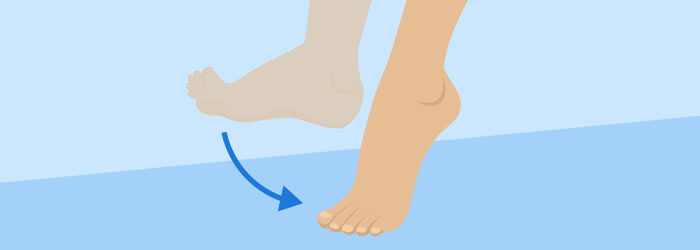
Those of us who help people recovering from stroke relearn to walk are always thinking about foot clearance during the swing phase of gait.
We always have to think about safety and we are fearful that foot drop will cause these individuals to drag their toes and perhaps fall while walking. This is the last thing we want! As a result, we focus on the most obvious problem (the foot clearance issue) and often make decisions about bracing without regard to the bigger picture – the long-term recovery of the patient.
When we make the decision to put a rigid orthosis on a patient, such as a solid-ankle foot orthosis (AFO), we certainly fix the supposed foot drop. However, we often not only immobilize the ankle, which limits the ankle from moving into normal range of motions, we unfortunately also promote atrophy of the plantar flexors.
Are Plantar Flexors or Dorsiflexors at Fault?
There is a growing amount of evidence that the plantar flexors– NOT the dorsiflexors – are the bigger problem after stroke.
We are just starting to understand the role of the plantar flexors in gait after stroke. For example, we know now that knee hyperextension – a common problem after stroke – is primarily the result of weakness in the plantar flexors!1 We used to think that this problem was caused by spasticity in the plantar flexors or weakness in the quadriceps but it turns out that it is WEAKNESS in the calf!
What is Foot Drop, Really?
Even more interesting, there is even a question about whether or not people with stroke actually have foot drop like we assume that they do.
One group of researchers asked the question if limb clearance problems after stroke are the result of dorsiflexion weakness (i.e. foot drop) or if there is another mechanism at work.2 Using very sophisticated methods, they found that dorsiflexion may not be the primary problem. Instead, plantar flexion weakness is a large contributor to limitations in knee flexion and secondarily hip flexion, which negatively impacts the swing phase of gait.
The result is that the weakness in the calf secondarily results in foot clearance problems. Who knew?
Focus Interventions on Plantar Flexors
The bottom line is that if we want to improve walking in people with stroke we may want to focus our efforts on the plantar flexors, not the dorsiflexors.
Allen et al.3 concluded that plantar flexor coordination (i.e. symmetry of forward propulsion when walking) is an indicator of recovery after stroke. People that failed to achieve this symmetry were classified as persons who had “compensated” after stroke as opposed to recovered.
In light of what we understand about neuroplasticity4, we are always interested in promoting recovery, when possible, rather than compensation.
- Cooper A, Alghamdi GA, Alghamdi MA, Altowaijri A, Richardson S. The relationship of lower limb muscle strength and knee joint hyperextension during the stance phase of gait in hemiparetic stroke patients. Physiotherapy research international : the journal for researchers and clinicians in physical therapy. Sep 2012;17(3):150-156.
- Little VL, McGuirk TE, Patten C. Impaired limb shortening following stroke: what's in a name? PloS one. 2014;9(10):e110140.
- Allen JL, Kautz SA, Neptune RR. Forward propulsion asymmetry is indicative of changes in plantarflexor coordination during walking in individuals with post-stroke hemiparesis. Clinical biomechanics. Aug 2014;29(7):780-786.
- Kleim JA, Jones TA. Principles of experience-dependent neural plasticity: implications for rehabilitation after brain damage. Journal of speech, language, and hearing research : JSLHR. Feb 2008;51(1):S225-239.









