Central Vestibular Recovery and Intervention: A Case-Based Review
Presented by Laura Morris and Jeffrey Hoder
12-Month Subscription
Unlimited access to:
- Thousands of CE Courses
- Patient Education
- Home Exercise Program
- And more
This course provides a comprehensive review of recovery and intervention strategies for central vestibular dysfunction, using case-based examples to guide practical application. Participants will explore the impact of conditions such as lateral medullary syndrome, vestibular migraine, and persistent postural-perceptual dizziness (PPPD) on gaze stability, postural control, and functional mobility. The course emphasizes evidence-based interventions, including sensory reweighting, habituation exercises, and aerobic conditioning, tailored to the unique needs of each patient. Designed for occupational and physical therapists, this course equips clinicians to improve patient outcomes by addressing complex vestibular impairments in diverse clinical settings.
Learning Objectives
- Analyze intervention strategies for addressing central and peripheral vestibular dysfunction to improve patient outcomes in clinical settings
- Apply general guidelines for vestibular rehabilitation to real-world cases involving central vestibular dysfunction, focusing on individualized patient care
- Modify intervention approaches based on clinical presentation and current evidence to address the specific needs of patients with central vestibular impairment
- Select appropriate intensity and duration of interventions by assessing pathology and disease progression, ensuring interventions support patients’ functional goals and roles within daily activities
Meet your instructors

Laura Morris
Laura Morris is a physical therapist and lecturer with more than 30 years of experience in the management of adults with neurologic disorders. Her clinical work focuses on vestibular disorders and mild traumatic brain injury at Elmhurst Hospital, part of Edward-Elmhurst Health in the Chicago area. She teaches continuing…

Jeffrey Hoder
Dr. Hoder’s specific area of expertise is in adult neurological rehabilitation related to the examination and management of adults with neurological deficits. As a clinician and educator, his philosophy is to train compassionate and critical physical therapy clinical scientists to evaluate and manage individuals with complex…
Chapters & learning objectives
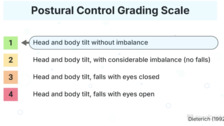
1. General Guidelines and PICA Stroke Case
This chapter introduces foundational principles for managing central vestibular dysfunction, such as static versus dynamic compensation and sensory reweighting. Through a case study of a patient with a PICA stroke and lateral medullary syndrome, participants will learn targeted strategies for addressing gaze instability, postural disorientation, and balance deficits. The integration of functional training with tools like body weight–supported treadmill training demonstrates how to enhance patient mobility and independence.

2. Cerebellar Dysfunction
This chapter focuses on cerebellar dysfunction, including the pathophysiology and rehabilitation of conditions such as cerebellar mass lesions and hydrocephalus. A case study of a patient recovering from hemangioblastoma surgery illustrates the challenges of addressing dynamic gaze stability, postural control, and functional mobility. Clinicians will gain strategies to manage cerebellar ataxia and vestibular impairments using habituation and balance-focused interventions.

3. Vestibular Migraine
In this chapter, participants will examine the complexities of vestibular migraine through a detailed case study. The chapter highlights the interplay between migraine triggers, visual motion intolerance, and functional impairments. Clinicians will learn to combine medical management with rehabilitation strategies such as aerobic conditioning, sensory reweighting, and vestibular habituation to support patient recovery and improve quality of life.

4. Concussion/PPPD Case, Summary, and Conclusions
This chapter explores the rehabilitation of patients with PPPD following traumatic brain injury or concussion. A case study details the impact of sensory hypersensitivity, chronic dizziness, and reduced confidence on functional mobility and social participation. Participants will learn to implement interventions focusing on grounding techniques, visual dependence reduction, and relaxation training, helping patients regain independence and return to meaningful activities.