Readiness Changes Everything: The First Step in Successful Pediatric Tube Weaning
Learn how to recognize true pediatric tube weaning readiness so you can confidently guide families toward safe, sustainable feeding progress. This article breaks down what matters most—before feeds are ever reduced.
December 17, 2025
9 min. read

When families come to me asking whether their child is ready to start tube weaning, they’re often eager and hopeful—but also overwhelmed. Many have been living in survival mode for months or even years. They want to move toward oral feeding, but they’re unsure where to start, what to look for, or how to know whether their child is truly ready.
Clinicians feel this uncertainty too. We all want to support our patients safely and effectively, yet the earliest step—recognizing readiness—is frequently misunderstood. In my work on our interdisciplinary tube-weaning team, I’ve learned that readiness isn’t a checklist or a quick assessment. It’s a multidimensional picture that shapes the entire trajectory of the weaning process.
In my course Pediatric Tube Weaning Part 1: The Role of the Feeding Therapist, I walk clinicians through this readiness framework in detail. In this article, I want to share a high-level look at the signs I consider first—long before we talk about decreasing feeds or building a therapy plan.
Why readiness matters more than motivation alone
Children can show interest in food long before they’re physiologically or emotionally ready to decrease tube feeds. A child might take small tastes, participate in family meals, or explore foods with their hands—but that alone doesn’t mean their system is prepared for a structured wean.
I frequently meet clinicians who feel “stuck” despite providing excellent therapy. They’re working on oral skills, sensory exploration, or mealtime routines, but progress stalls. Often, it’s not because therapy isn’t working. It’s because the child wasn’t truly ready—medically, developmentally, or emotionally—to take the next step.
Recognizing readiness protects the child’s safety, supports their hunger and comfort, and allows the feeding therapist to move forward with confidence. It also helps caregivers understand the purpose behind each step, reducing stress and fear in the process.
The four high-level domains of tube-weaning readiness
While every child’s situation is unique, readiness generally emerges across four broad domains. These categories help guide my thinking before I consider any structured reduction in tube feeds.
1. Medical and physiological foundations
A child’s medical picture plays a major role in whether we can begin tube weaning. When underlying conditions such as reflux, motility challenges, constipation, or food intolerances are not well managed, eating can feel uncomfortable—often affecting appetite, hunger cues, or interest in oral intake. Upcoming surgeries or progressive diagnoses can also influence timing of weaning or the decision for tube removal. Sometimes, a child is medically ready to increase their oral intake but not yet ready to have their tube removed.
Growth patterns are also part of this picture. Young children don’t grow linearly,1 and caregiver insight into appetite, preferred foods, and daily intake often provides meaningful context. What matters most is understanding whether the child’s overall medical status supports safe, sustainable progress—not whether growth appears perfectly consistent at every point in time.
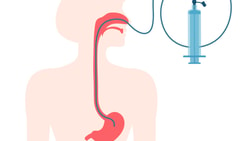
2. Safe swallowing and oral feeding skills
Before we reduce tube feeds, I want to feel confident that a child can safely swallow the textures they are being offered. An instrumental assessment, such as a videofluoroscopic swallow study (VFSS) or fiberoptic endoscopic evaluation of swallowing (FEES), is not always required but may be indicated if concerns arise regarding swallow safety as oral intake increases.
Safety is dynamic. As children grow, develop new skills, and participate more consistently in meals, their ability to manage a variety of consistencies and textures evolves. Sometimes readiness simply requires time—time for observation, monitoring, and building trust with the child and their caregivers.
3. Developmental skill and endurance readiness
Eating is physical work, and children need the endurance and coordination to consume meaningful volumes by mouth. For children with low tone or complex medical conditions, this can be especially challenging.
Skills do not need to be perfect—many develop throughout the weaning process—but a child should have a baseline ability to manage tastes or small volumes, prior to beginning tube weaning. Often, developmental stage, not chronological age, guides expectations. An older child may still begin with purées if that aligns with their current skill level. Meeting a child where they are is a crucial part of recognizing readiness.
4. Caregiver and environmental readiness
This domain is often the most overlooked, yet it’s one of the most important.
Families bring their own lived experiences into the tube-weaning process. Some caregivers describe grieving the loss of the feeding experience they imagined and the significant lifestyle and emotional shifts that come with caring for a medically complex patient.1,2
These experiences shape how ready a family feels. Stress, fear, or past trauma can make any change feel threatening. This is where family-centered care comes in to help create the safety and partnership needed to move forward. Respectful communication, shared information, and collaborative goal-setting support caregivers in feeling informed and involved.3,4
How tube feeding schedules shape readiness
How tube feeds are scheduled—and how nutrition is delivered throughout the day—strongly influences a child’s hunger cues, appetite rhythm, and interest in oral intake. Children receiving continuous feeds, for example, may have very few natural opportunities to experience hunger or develop internal motivation to eat.
Certain tube feeding schedules can limit appetite conditioning. Continuous feeds may suppress hunger signals, while bolus or overnight schedules can create more predictable windows for hunger to emerge. Feeding schedule (continuous vs. bolus vs. overnight), formula type, and caloric density all influence how full a child feels and how motivated they are to engage in mealtimes.
These factors don’t determine readiness on their own, but they help clinicians understand what the child’s body experiences each day and how hunger and fullness are interpreted. In the course, I explain how feeding schedules are adjusted in collaboration with the medical team, but at a high level, what matters most is this: feeding schedules shape how we observe, support, and interpret readiness for tube weaning.
The emotional layer: why family readiness cannot be overlooked
Every tube-weaning journey begins with the family—and their emotions matter just as much as the child’s skills.
Caregivers often carry a mix of emotions shaped by years of complex feeding experiences. Many of the families I work with describe:
fear of weight loss
anxiety around aspiration
guilt from past feeding struggles
feeling judged by medical teams
worry that they’re “not doing enough”
These emotions don’t mean a family is unprepared. They mean they’re human.
Temporary weight changes, for example, are common—and expected. Most children in the process of tube weaning experience some degree of weight loss, yet this does not predict slowed long-term growth.5 Sharing this context can help lessen fear and build trust.
Families also carry the weight of lived experience. Insufficient weight gain in the past may have triggered medical pressure, contributing to caregiver stress and, at times, increased pressure on the child. Many parents also describe grieving the loss of the feeding experience they imagined—the routines, connection, and sense of control they hoped for. When medical experiences have been difficult or traumatic, it’s understandable that caregivers may feel cautious or afraid to change anything.
This is where family-centered care becomes essential. Respectful, collaborative conversations help align caregiver and clinician goals, even when those goals do not perfectly match at the beginning. Core principles such as respect, dignity, information sharing, and authentic participation provide a strong foundation for building caregiver confidence.
Caregiver education also takes time. Small, manageable pieces of information offered steadily over time can help caregivers build trust in both the process and in themselves.
When families feel heard, supported, and included in decision-making, readiness becomes a shared foundation—not a source of stress. Tube weaning is not something done to families. It’s something we do with them.
What happens after readiness is established
Recognizing readiness is only step one. Once a child and family demonstrate readiness, our work shifts toward:
structuring positive mealtime environments
supporting sensory and oral-motor skill development
collaborating with the gastroenterology team, dietitians, and psychologists
monitoring safety, hydration, endurance, and skill progression
helping caregivers navigate plateaus, regressions, and obstacles
These next steps require careful planning, collaboration, and ongoing clinical reasoning. In Part 1 of the course, I explain how these elements fit together. In Pediatric Tube Weaning Part 2: Learning From Case Studies, I demonstrate how readiness transitions into real-world weaning journeys.
Readiness is the foundation of tube-weaning success
Recognizing readiness is a clinical skill, an observational skill, and—perhaps most importantly—a relational skill. When we understand the full picture of a child’s medical status, safety, developmental abilities, and family experience, we can make informed decisions that support safe, meaningful progress.
If you’d like to learn more about how to assess readiness, collaborate with an interdisciplinary team, support skill development, and work through real-world challenges, I invite you to explore the Pediatric Tube Weaning course series:
Tube weaning is complex—but with thoughtful preparation and compassionate guidance, it can also be a deeply rewarding journey for children, caregivers, and clinicians.
For clinicians working with thickened liquids during pediatric feeding and swallowing care, you may also be interested in:
References
Dunitz-Scheer, M., & Scheer, P. J. (2022). Child-led tube-management and tube-weaning. Springer Nature Switzerland AG. https://doi.org/10.1007/978-3-031-09090-5
Hewetson, R., & Singh, S. (2009). The lived experience of mothers of children with chronic feeding and/or swallowing difficulties. Dysphagia, 24(3), 322–332. https://doi.org/10.1007/s00455-009-9210-7
Lively, E. J., McAllister, S., & Doeltgen, S. H. (2023). Parents’ experiences of their child’s transition from tube to oral feeding during an intensive intervention programme. Child: Care, Health and Development, 49(4), 740–749. https://doi.org/10.1111/cch.13061
Johnson, B. H., & Abraham, M. R. (2012). Partnering with patients, residents, and families: A resource for leaders of hospitals, ambulatory care settings, and long-term care communities. Institute for Patient- and Family-Centered Care.
Wright, McNair, S., Milligan, B., Livingstone, J., & Fraser, E. (2022). Weight loss during ambulatory tube weaning: Don’t put the feeds back up. Archives of Disease in Childhood, 107(8), 767–771. https://doi.org/10.1136/archdischild-2021-322686
Below, watch Allison Brown discuss swallow safety in pediatric tube weaning in this brief clip from her Medbridge course "Pediatric Tube Weaning Part 1: The Role of the Feeding Therapist."