Reducing Readmissions Part 3: Social Determinants of Health
Presented by Colleen Morley
12-Month Subscription
Unlimited access to:
- Thousands of CE Courses
- Patient Education
- Home Exercise Program
- And more
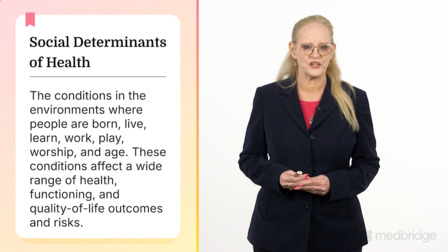
This course explores how social determinants of health (SDOH) critically influence hospital readmission risk and outlines equity-focused strategies to mitigate these risks. The core message is that factors like economic stability, housing, transportation, and health literacy account for a large percentage of health outcomes, and preventing readmissions requires moving beyond clinical readiness to address a patient’s real-world readiness through tools, such as the Patient Activation Measure (PAM), the teach-back method, and motivational interviewing (MI), and the use of community health workers (CHWs). The SAFEDC model is presented as a structured framework for ensuring equitable transitions of care by integrating socioeconomic screening, activation, follow-up, education, discharge readiness, and consistency into the process.
Learning Objectives
- Describe how social determinants of health (SDOH) influence hospital readmission risk
- Identify strategies for improving health literacy and addressing access-related barriers
- Discuss the role of implicit bias and health equity in readmission prevention programs
- Apply community-based and patient-centered interventions to mitigate SDOH risks
- Utilize patient activation and motivational interviewing to support self-management
Meet your instructor

Colleen Morley
Dr. Colleen Morley has held positions in acute care as director of case management at several acute care facilities and managed care entities in Illinois, overseeing utilization review, case management, and social services for more than 12 years and piloting quality improvement initiatives focused on readmission reduction and…
Chapters & learning objectives

1. Understanding Social Determinants of Health and Readmission Risk
The course begins by defining SDOH as conditions in the environments where people live, work, and age, highlighting their central role in readmission risk assessment, as they account for 80% of health outcomes.
2. Health Literacy, Implicit Bias, and Equity in Care
Chapter 2 details how low health literacy and provider implicit bias contribute to poor postdischarge outcomes, advocating for universal precautions like the teach-back method and a shift from assessing clinical readiness to real-world readiness.

3. Access to Care, Patient Activation, and Community Resources
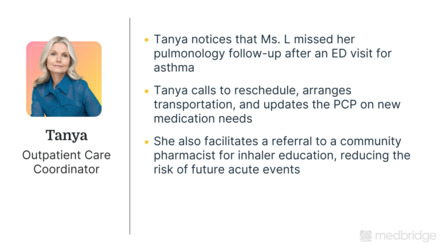
Chapter 3 presents high-impact strategies like the Patient Activation Measure (PAM) to gauge a patient’s readiness for self-management, the use of community health workers (CHWs) to close social care gaps, and motivational interviewing (MI) to resolve ambivalence and foster self-management.

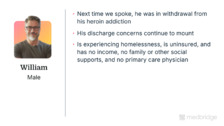
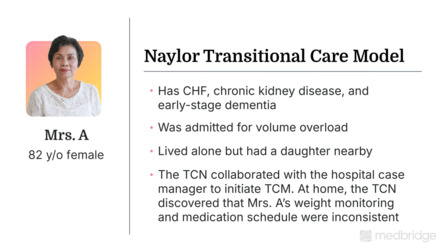
4. Case Studies and Equity-Focused Readmission Programs
This chapter illustrates how equity-focused models, such as the SAFEDC framework, which standardizes SDOH screening and follow-up, disrupt the cycle of readmissions and shift the narrative from patient "noncompliance" to addressing systemic and social barriers.
5. Question and Answer Session
In this chapter, Colleen Morley will address common questions about reducing readmissions.
More courses in this series

Reducing Readmissions Part 1: Understanding the Landscape
Colleen Morley
Reducing Readmissions Part 2: Evidence-Based Strategies
Colleen Morley
Reducing Readmissions Part 3: Social Determinants of Health
Colleen Morley
Reducing Readmissions Part 4: The Case Manager’s Role
Colleen Morley

Reducing Readmissions Part 5: Best Practices and Future Directions
Colleen Morley