5 Steps to Advancing Physical Therapy for Stroke Patients at Home

For many clinicians, developing and progressing physical therapy for stroke patients at home can feel like a daunting task. But having a process to work from can help increase your efficiency, boost your confidence, and improve outcomes. In this article, we’ll provide a step-by-step process for advancing home exercise programs (HEPs) specifically tailored for stroke recovery.
Understanding the Needs of Post-Stroke Patients
When working with post-stroke patients, it is essential to recognize their unique rehabilitation needs. Physical therapy for stroke patients at home focuses on restoring mobility, strength, and function lost due to stroke. The exercises and strategies outlined here are designed to address the specific challenges faced by these patients, helping them regain independence in their daily activities. Tailoring HEPs to post-stroke patients ensures that therapy is not only effective but also manageable for both patients and their caregivers.
Step 1: Gather Information
First, it’s important to gather information that will assist you in developing a suitable physical therapy for stroke patients at home program that won’t overwhelm your patient or their caregiver. You’ll want to:
- Ask your patient and the primary caregiver(s) what two functional activities are most frustrating to them daily and would make the biggest impact if the patient were able to complete them with less difficulty. (These may change continually as the patient improves, but stay focused.)
- Determine what barriers are impacting performance or completion of these tasks.
- Decide on the two most important areas for the patient to improve while performing the functional task. You’ll want to be task specific and allow as many repetitions as possible while addressing those primary limitations.
- Identify the primary impairments (for example, isolated active movement of the arm or lack of gluteus medius strength) impacting the patient’s ability to perform daily activities such as standing up and pulling up their pants, putting on their shirt, and maintaining their balance standing in the bathroom.
Step 2: Assess
Imagine that your patient requires moderate assistance with turning in the bathroom during activities-of-daily-living (ADL) tasks. Observation is key! Take a look at the following:
- What does your patient look like when they’re turning? Are they stable in the pelvis to allow shifting of the weight? Possible assessment: gluteus medius weakness.
- Are their eyes moving appropriately during movement? Possible assessment: eye tracking issue.
- Are they collapsing in the trunk? Possible assessment: proximal weakness in the trunk.
- Are they flexed over and relying heavily on their upper extremities to stay upright? Possible assessment: gluteus maximus weakness.
- Do they lose balance instantly if their eyes are closed? Possible assessment: decreased somatosensory function.
Step 3: Intervene
When working on functional tasks in the clinic, make adjustments that will target the impairments in your hypotheses above.
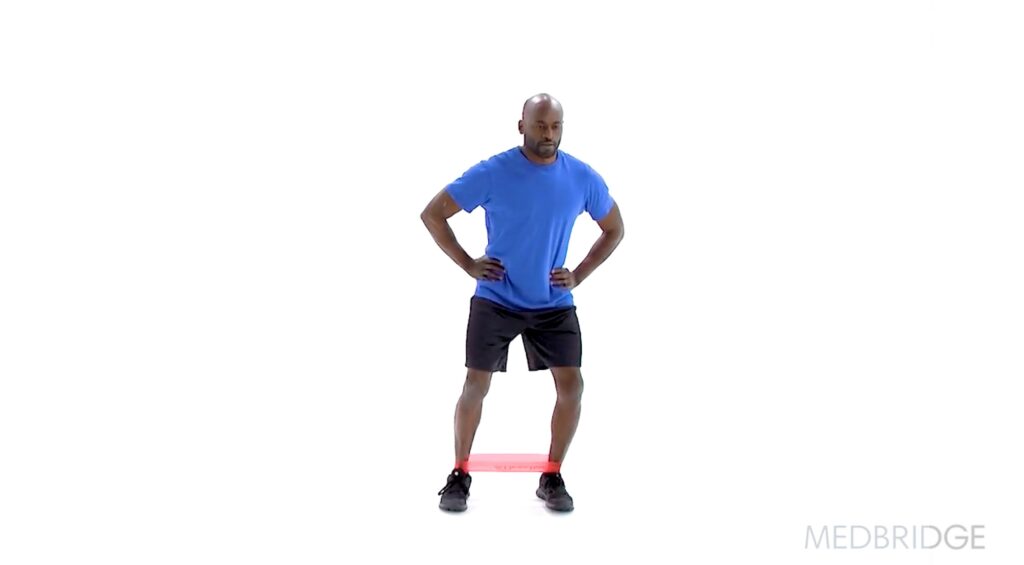
Addressing Gluteus Medius Weakness
Add a resistance band around the legs during sit-to-stand or standing activities to increase gluteus medius activation.
Addressing Eye Tracking Issues
Do prepping with visual tracking activity or smooth pursuits to prepare the visual motor and/or vestibular systems.
![]()
Addressing Trunk Weakness
Add sustained pushing to increase trunk activation for proximal weakness.

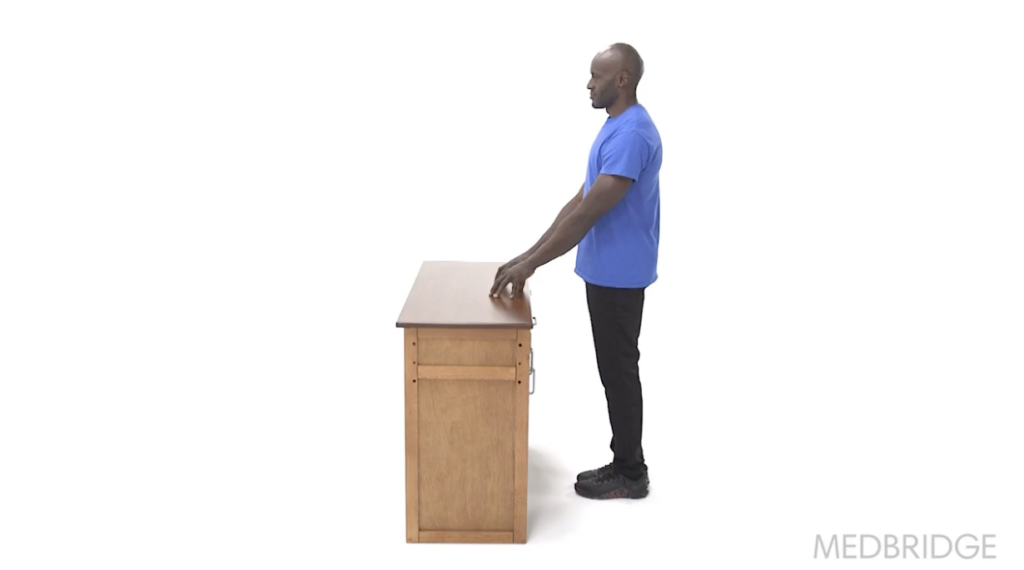
Addressing Decreased Somatosensory Function
Perform standing balance tasks at the counter with eyes closed to improve somatosensory function.
Step 4: Develop Your HEPs
Adjust your home program to address any one of these impairments or limitations. This will allow you to provide increased challenge during therapy sessions without overwhelming your patient.
Step 5: Follow Up
Regularly perform informal reassessments to modify the HEP as the patient progresses. It’s essential to remove older tasks and introduce higher-level ones to keep the patient from feeling overwhelmed with too many exercises, ensuring the effectiveness of physical therapy for stroke patients at home.
Empowering Recovery Through Structured Home Programs
Advancing physical therapy for stroke patients at home requires a thoughtful and individualized approach. By following these five steps—gathering information, assessing patient needs, implementing targeted interventions, developing tailored home exercise programs, and regularly following up—you can enhance the recovery process for your post-stroke patients. These strategies not only address specific impairments but also empower patients and their caregivers to actively participate in the rehabilitation journey. With a well-structured plan, you can provide effective, manageable, and impactful home programs that foster independence and improve quality of life for stroke survivors.

