Manual Treatment for Lower Quadrant Asymmetries, Movement Dysfunction, and Pain

What role do asymmetries of the lower quadrant play in movement dysfunction? What evidence-based and innovative assessments and interventions are available to effectively treat your patients and athletes with lower quadrant dysfunction?
Emerging evidence suggests that lower quadrant asymmetries increase the risk of injury and are related to a number of conditions that cause pain and movement dysfunction in our patients and athletes.1, 2, 3
Test/Treat/Retest

Test/Treat/Retest
The Test/Treat/Retest philosophy is helpful when working with patients and athletes. Accurate assessments should be selected to drive effective interventions. Retesting allows you to better identify whether the applied interventions have been effective and whether additional or alternate treatments should be included.
In the clip below, I identify evidence-based Graston Technique® assessments that will enhance your ability to select effective interventions.
Including Manual Therapy in Your Treatment
Graston Technique® Manual Therapy
What interventions do you typically use to alleviate pain and movement dysfunction in the lower quadrant? Do you know the proposed mechanisms of effectiveness behind the interventions you use with your patients or athletes? Is manual therapy, and specifically instrument-assisted soft tissue mobilization (IASTM) via the Graston Technique, even effective?
Current evidence indicates that manual therapy, regardless of the techniques selected, is effective due to largely neurophysiological mechanisms.4 Appropriate manual therapy techniques can influence pain, mobility, and motor control, which in turn leads to improved movement efficiency and function.
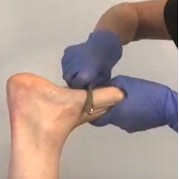
In the following clip, I demonstrate a manual therapy technique that combines IASTM via the Graston Technique and joint mobilization to positively influence pain, mobility, and function to the first metatarsophalangeal (MTP) joint.
Adding a Customizable System of Orthotics to Your Practice

Fitting Customizable Orthotics
The effectiveness of custom orthotics has been challenged in the literature. Additionally, clinicians tend to experience frustration when dealing with the expense and lengthy fabrication process required when using an orthotic lab.
Current research indicates, however, that customizable orthotics can be effective when treating lower quadrant diagnoses, such as patellofemoral pain and plantar fasciosis, and to prevent injuries.5, 6, 7 A customizable system of orthotics can add additional neurophysiological input when patients experience these types of conditions. Additionally, they can be fabricated right in your clinic or training room in just one or two sessions at a reasonable cost to your patients and athletes.
In the following clip, I fit my patient with an in-office fully customizable orthotic.
You can learn more about this approach to lower quadrant movement dysfunction—along with assessment and treatment techniques to relieve pain and get your patients and athletes back in the game—in my MedBridge course, “Graston Technique®: Evidence-Based Management for the Lower Quadrant.”
- Benca, E., Listabarth, S., Flock, F. K. J., Pablik, E., Fischer, C., Walzer, S. M., Dorotka, R., Windhager, R., & Zial, P. (2020). Analysis of running-related injuries: The Vienna Study. Journal of Clinical Medicine, 9(2), 438. https://doi.org/10.3390/jcm9020438
- Tanamas, S., Hanna, F. S., Cicuttini, F. M., Wluka, A. E., Berry, P., & Urquhart, D. M. (2009). Does knee malalignment increase the risk of development and progression of knee osteoarthritis? A systematic review. Arthritis and Rheumatism, 61(4), 459–57. https://doi.org/10.1002/art.24336
- Amraee, D., Alizadeh, M. H., Minoonejhad, H., Razi, M., & Amraee, G. H. (2017). Predictor factors for lower extremity malalignment and non-contact anterior cruciate ligament injuries in male athletes. Knee Surgery, Sports Traumatology, and Arthroscopy, 25(5), 1625–1631. https://doi.org/10.1007/s00167-015-3926-8
- Bialosky, J. E., Beneciuk, J. M., Bishop, M. D., Coronado, R. A., Penza, C. M., Simo, C. B., & George, S. Z. (2018). Unraveling the mechanisms of manual therapy: modeling an approach. Journal of Orthopaedic and Sports Physical Therapy, 48(1), 8–18. https://www.jospt.org/doi/10.2519/jospt.2018.7476
- Martin, R. L., Davenport, T. E., Reischl, S. F., McPoil, R. G., Matheson, J. W., Wukich, D. K., McDonough, C. M., Altman, R. D., Beattie, P., Cornwall, M., Davis, I., Dewitt, J., Elliott, J., Irrgang, J. J., Kaplan, S., Paulseth, S., Torburn, L., Zachazewski, J., & Godges, J. J. (2014). Heel pain—plantar fasciitis: Revision 2014. Journal of Orthopaedic & Sports Physical Therapy, 44(11), A1–A33. https://www.jospt.org/doi/10.2519/jospt.2014.0303
- Landorf, K. B., Keenan A., & Herbert, R. D. (2006). Effectiveness of foot orthoses to treat plantar fasciitis: A randomized trial. Archives of Internal Medicine, 166(12), 1305–1310. doi:10.1001/archinte.166.12.1305.
- Franklyn-Miller, A., Wilson, C., Bilzon, J., & McCrory, P. (2011). Foot orthoses in the prevention of injury in initial military training: A randomized controlled trial. The American Journal of Sports Medicine, 39(1), 30–37. https://doi.org/10.1177/0363546510382852