The Future of Physical Therapy Is Hybrid: An Interview With Ivy Rehab on Digital MSK Care

During a recent webinar, MedBridge sat down with Jonathan Jean-Pierre, COO of Ivy Rehab, to discuss Ivy’s hybrid approach to physical therapy, which is centered on the philosophy that in-person care and the provider-patient relationship are still critical to patient success.
In this article, we’ll explore how organizations like Ivy Rehab are using a hybrid care model to expand access to therapy and drive ongoing engagement with patients.
Musculoskeletal (MSK) Conditions in the US Are Prevalent and Have a High Economic Toll
- More than 50 percent of adults over the age of 18, approximately 124 million people, have reported a musculoskeletal condition per year, and that number rises to nearly 75 percent for adults ages 65 and over.1
- The estimated national cost of musculoskeletal pain in the USA is $560–$635B.2
- According to CMS 2023 National Health Expenditure (NHE) Fact Sheet, the NHE grew 4.1% to $4.5 trillion in 2022, or $13,493 per person.
- 12-14% of all healthcare spending went to MSK care.3
- By 2030, all 73 million Baby Boomers will be Medicare-eligible.4
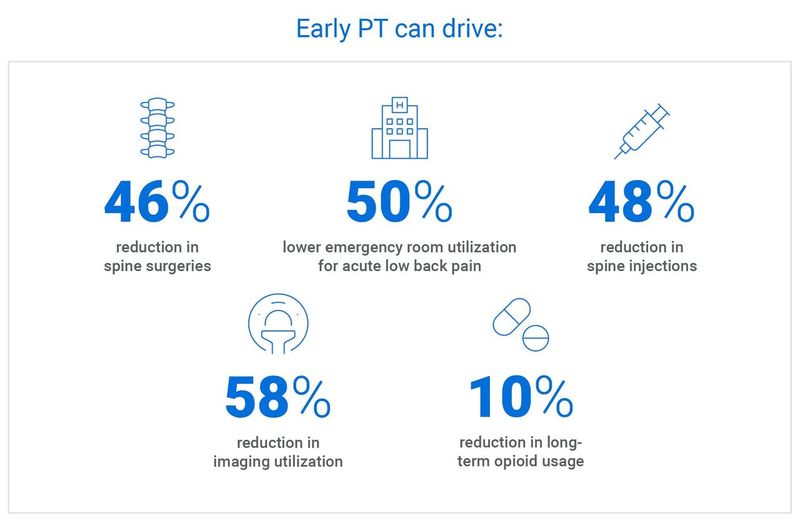
Something must change—and soon—before the problem turns into a crisis that our overburdened system can’t handle. But there’s strong evidence for one modality of care: early physical therapy.
If early physical therapy is so effective, why isn’t it the standard? Unfortunately, it’s not so simple to achieve because of the limitations of the two most prominent PT models: in-clinic physical therapy and digital-only physical therapy. And while the increase in MSK volume presents an opportunity to boost the value of PT, providers will need to adjust their practices to be able to overcome these limitations and capture this opportunity.
Current Physical Therapy Models and Their Limitations
In-Clinic Physical Therapy
In-clinic PT is the most common way for patients to obtain therapeutic care today, and has been proven again and again to be highly effective. But this model also comes with a number of significant challenges, the most common of which are access and adherence.
- A massive number of patients require MSK each year (as highlighted before), but the current in-clinic system couldn’t handle the massive caseload.
- According to industry statistics, fewer than 70 percent of patients actually complete their full course of care.7
- Common barriers like transportation, work schedule, or arranging child care; as well as patients living in rural areas where fewer services are available.
Digital-Only Physical Therapy
Digital-only PT slowly gained prominence in the past decade before taking a lightspeed jump forward during the COVID-19 pandemic. Telehealth, remote patient monitoring, digital HEP, and patient education—these critical tools have been instrumental in solving some of the access and adherence problems facing patients using in-clinic PT. It does, however, come with its own set of downsides—notably enrollment and impact of outcomes.
- Digital-only MSK solutions disintermediate the in-clinic providers. While digital MSK care is great for increasing access, there’s no substitute for high-quality provider-led therapy.
- Higher-acuity patients require hands-on care and also drive the most cost to the healthcare system. Without the right level of care, this patient population will likely end up in more cost-intensive specialty services instead of early therapy.
Both models have their pros and cons, but ultimately neither will be able to keep up with the high demands of today’s healthcare landscape. There is, however, good news: By adopting a hybrid care model, we can ensure both better access and quality of care.
The Future of Physical Therapy Is Hybrid Care
A hybrid care model takes the best aspects from both in-clinic PT and digital PT and combines them into a single, highly effective care program. In hybrid care, organizations can create a layer of digital technology that spans the entire patient journey. Virtual care consultations can be offered as a standalone option or as a supplement to in-person care, making these ideal for low-risk interventions as well as check-ins. Once a patient is in the system, digital tools like virtual care visits, remote monitoring, patient messaging, and patient portals provide new opportunities for engagement.
By using digital care to expand treatment options, you can continue to treat, engage, and inform patients even when they aren’t able to physically make it for an in-person session. With the time saved from this increased efficiency, clinicians can see more patients and spend more hands-on time with higher acuity patients who need the most care. And because patients get their consultations faster, triage is more effective, directing higher acuity patients to the in-person care they need earlier in the process, while lower-acuity patients receive guidance to get them started on a home program or in-person care. You can serve more patients, more efficiently—they get better faster, and you don’t lose them to other providers.
How MedBridge Pathways Can Help You Benefit From Hybrid Care
MedBridge Pathways is our new digital care platform, purpose-built to keep therapy at the forefront of care and help organizations deliver superior patient outcomes across the musculoskeletal care spectrum. By supplementing existing in-person programs with a variety of digital care pathways based on patient acuity, Pathways provides a solution that engages the patient with therapy-driven care that incorporates their condition and lifestyle, and delivers that valuable data back into the clinician’s hands so they can leverage their expertise.
Programs are personalized through an onboarding questionnaire that takes into account patients’ pain, goals, and activity levels.Patients are guided through exercises by evidence-based progression criteria in multiple phases:
- Engaging video, text, and interactive education provide a guide for the patient, supporting them throughout their rehab journey.
- Gamification and data-driven progress tracking motivate patients to complete their program.
- Periodic surveys and PROs are collected to help measure progress, identify red flags, and manage progression.
MedBridge Pathways won’t disrupt the clinician-patient relationship; instead, it empowers providers to keep patients in their ecosystem for a lifetime of care. Providers can supplement brick-and-mortar care with a cutting-edge, digitally-enabled therapy platform that provides patients a modern, convenient care experience, improves health outcomes, and allows higher care capacity while reducing the provider workload.
MedBridge Pathways is now in beta testing and will open to early adopters in 2024. Request a meeting to find out how you can join the digitally-enabled future of MSK care: provider-first, therapy-driven care for patients across the care continuum.
About Ivy Rehab
Founded in 2003, Ivy Rehab is a rapidly growing network of best-in-class outpatient physical, occupational, speech, and ABA therapy clinics. The Ivy Rehab Network consists of multiple brands dedicated to providing exceptional care and personalized treatment to get patients feeling better, faster. With backing from leading middle-market private equity firm Waud Capital Partners, Ivy Rehab will continue to grow and further expand its U.S. footprint.
- BMUS Impact of MSK on Americans booklet_4th Edition (2018).pdf (boneandjointburden.org); BMUS: The Burden of Musculoskeletal Diseases in the United States | Prevalence, Societal and Economic Cost (boneandjointburden.org); 2015
- Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain. 2012 Aug;13(8):715-24. doi: 10.1016/j.jpain.2012.03.009. Epub 2012 May 16. PMID: 22607834.
- CMS 2023 National Health Expenditure (NHE) Fact Sheet
- https://www.forbes.com/sites/deborahwince-smith/2022/02/25/bracing-for-the-silver-tsunami/?sh=163bbaa633e
- https://www.hopkinsmedicine.org/news/newsroom/news-releases/early-physical-therapy-associated-with-less-health-care-resource-use-for-patients-with-acute-lower-back-pai
- https://med.stanford.edu/news/all-news/2018/12/early-physical-therapy-can-reduce-risk-of-long-term-opiod-use.html
- AHRQ Medical Expenditure Panel Survey, 2015


 Source: Citation
Source: Citation 

