4 Tips to Maximize Home Exercise Program Participation

Participation in a home exercise program (HEP) outside the clinic or training facility can be a substantial factor in a patient’s positive and sustained long-term outcome. The following evidence-based tips can help achieve increased patient buy-in and adherence.
1. Provide Written and/or Video Instruction
Providing verbal instructions for your patients’ home exercise program is important, but if you’re not providing visual aids and/or videos, you’re losing quality and adherence. Pictures and videos, like the examples below, give clearer performance instructions than words alone. At least one study showed that patients receiving additional written and illustrated instruction had a 77.4% adherence rate vs the verbal instruction only group’s adherence rate of 38.1%.1 This is no surprise considering reports estimate that patients retain only 40-80% of medical information from a visit, and of the retained information, only 50% is correct.2
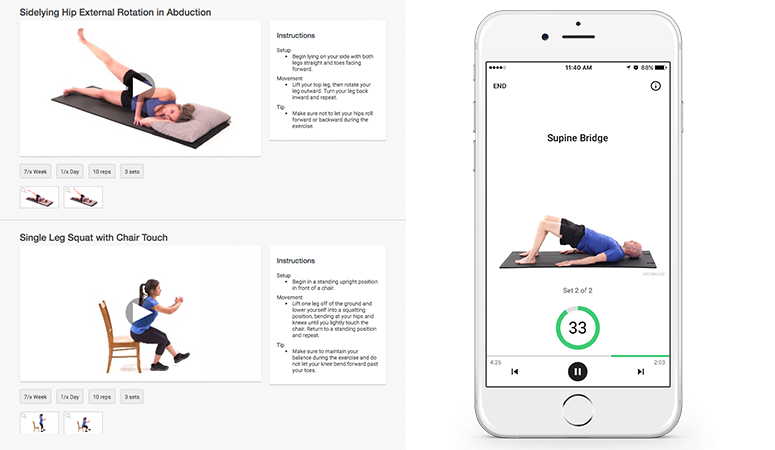
Below is an example of both a web-based (on the left) and an app-based HEP (on the right). It is important to provide the HEP in your patient’s preferred medium: print, email, text, or app. The MedBridge HEP Builder and Patient Mobile App can provide programs in any of these formats.
2. Less Is More
How many exercises do you give your patients on average? Evidence suggests that HEP adherence and performance inversely relates to number of exercises prescribed; meaning the greater number of exercises prescribed, the lower the adherence rate.3,4 For example, a group of military-based patients demonstrated increased adherence to a three exercise HEP vs a five exercise HEP.3 Another study showed that a in a >65 year old population, a group prescribed two exercises performed better than a group prescribed eight exercises (there was no difference between the five exercise group).4 This question definitely needs additional study, but it suggests HEP prescription efficiency is beneficial.
3. Exercise History is Key for HEP Prescription
Know your patient. Are you treating an elite athlete, a weekend warrior, a mother of three who works full time, or a sedentary person? The weekend warrior with a good exercise background will likely be more adherent to the a robust and comprehensive HEP while your sedentary client may need a simpler program. The history allows you to apply your clinical judgement to the HEP size noted above.
4. Make Your HEP Evolve
As healthcare reform lumbers forward, the number of available treatment sessions is decreasing, so the HEP definitely needs to serve as a primary intervention that grows and evolves throughout the episode of care. You should provide an HEP as early as possible and update it as your patient progresses. MedBridge can easily track your HEP in your EHR and updates can be made quickly with the individualized access codes. If your patient has the app or web-based HEP access, the HEP will update as soon as you save the program.
Putting these four steps together can lead to more efficient and more effective HEP. Plus, with tools like the MedBridge HEP Builder and corresponding Patient Mobile App, it’s easier now more than ever to create programs that make a difference for your patients.
- Schneiders, A. G., M. Zusman, and K. P. Singer. "Exercise therapy compliance in acute low back pain patients." Manual Therapy 3.3 (1998): 147-152.2.
- Kessels, Roy PC. "Patients’ memory for medical information." Journal of the Royal Society of Medicine 96.5 (2003): 219-222.
- Eckard, Timothy, et al. "Home exercise program compliance of service members in the deployed environment: an observational cohort study." Military medicine 180.2 (2015): 186-191.4.
- Henry, Kristin D., Cherie Rosemond, and Lynn B. Eckert. "Effect of number of home exercises on compliance and performance in adults over 65 years of age." Physical Therapy 79.3 (1999): 270-277.