The CMS Final Rule, VBP, and COVID-19 Vaccine Mandate: The Impact on Your Agency and How Healthcare Technology Can Help

It’s official: There’s a lot going on right now for home health and hospice organizations, from CMS implementing the COVID-19 vaccination mandate for Medicare and Medicaid providers, to releasing its final rule for 2022 and launching the Home Health Value-Based Purchasing Agreement (VBP).
Through all of this, agencies are being asked to perform better by improving quality of care while reducing costs. Yet many agencies have already been facing staffing challenges that may become worse with upcoming vaccine mandates.
To adapt well to these changes in the industry, it’s essential for agencies to boost staff retention through better engagement, reduce additional burnout on staff members, enhance clinical efficiency through high-quality training and onboarding, improve patient management, and overall find ways to do more with less.
In this article, we’ll take a look at some of the key aspects of the CMS final rule for 2022, VBP, and the CMS vaccine mandate, including:
- What they mean in a nutshell.
- The impact on your agency.
- How you can address them with healthcare technology.
Expansion of Home Health Value-Based Purchasing
As part of CMS’s final rule for 2022, CMS is moving forward with its plan to expand the Home Health Value-Based Purchasing Model (HHVBP), with a payment adjustment capped at 5 percent. The first performance year for the expanded model is 2023, providing agencies a one-year pre-implementation period to prepare. HHVBP is a major step forward in value-based care and links reimbursement to the quality of care delivered.
The impact:
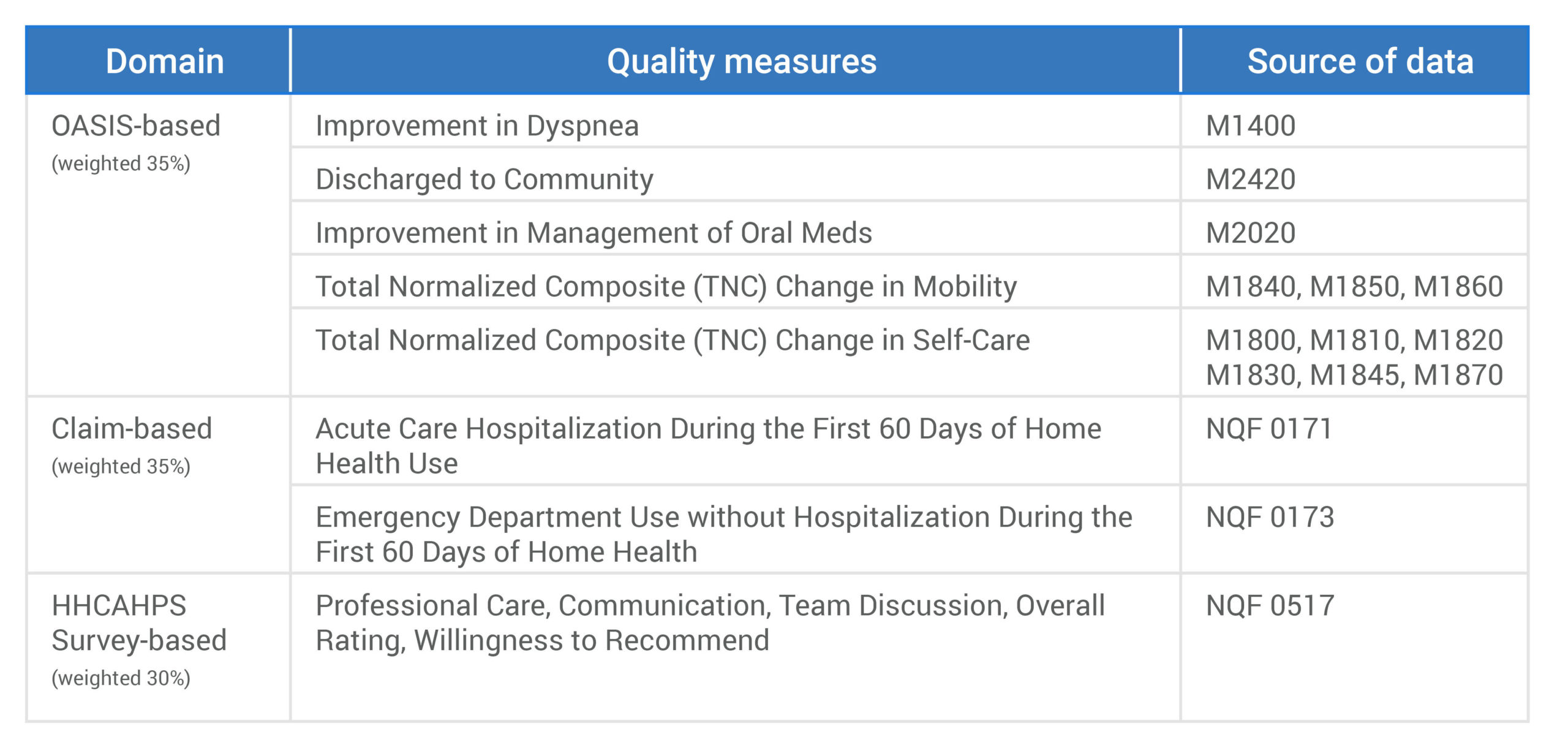
There is now a 5 percent plus or minus rate adjustment based upon the quality of care delivered starting in 2023 (with 2023 quality scores impacting payment rates starting in 2025). According to CMS, the model has resulted in an average 4.6 percent improvement in home health agencies’ quality scores as well as average annual savings of $141 million to Medicare. Your score is determined by the following:
- 35 percent of the quality score is based upon OASIS accuracy.
- 35 percent of the score will be based upon submitted claims for ED visits, as well as hospitalizations that occur within the first 60 days of a patient on service.
- 30 percent of the score will be based on the HHCAHPS survey.
What you can do:
Enhance your performance improvement plan. Developing, implementing, and maintaining an effective QAPI program will be essential for agencies shifting to HHVBP and those already operating under the model. While most agencies already closely monitor their quality outcomes, targeted performance improvement projects require additional guidance and best practice recommendations for implementation.
Reduce unnecessary visits and cost per episode with effective patient management. Providing the right care for the right patient at the right time is one of the most effective ways to provide effective, cost-efficient care, but keeping your patient engaged and activated in between visits is an ongoing challenge. By combining digital healthcare tools with patient education and staff training, you can replace and supplement costly in‑person visits, develop standardized care pathways, and implement best practices to keep your patients engaged and healthy.
Provide targeted, efficient OASIS training. To succeed under the HHVBP model, agencies will need to ensure accurate and complete documentation, and help staff understand the impact it can have on quality measures. Effective training and management tools are two of the most effective ways to establish a strong foundation for accurate OASIS data collection.
Occupational Therapists Allowed to Open Home Health Cases
Included in the final rule, occupational therapists (OTs) are now allowed to perform initial and comprehensive assessments for Medicare patients when:
- Occupational therapy is on the home health plan of care, with either physical therapy or speech therapy, and
- Skilled nursing services are not initially on the plan of care.
The impact:
While not permanent, this policy ensures timely delivery of home health care. As agencies continue to struggle with maintaining clinical capacity, this ruling assists in permitting another licensed provider to make timely OASIS visits. This policy helps improve your agency’s capacity for patient care and can also improve the timeliness in which cases are open.
What you can do:
Make sure your OTs are formally trained on OASIS. Not only is this essential to their role in initial and comprehensive assessments, but understanding the framework of OASIS can help your staff ensure quality care.
Survey Enforcement Requirements of Hospice
Medicare has said that it is finalizing changes to increase and improve transparency, oversight, and enforcement for hospice programs “in order to enhance the survey process by requiring the use of multidisciplinary survey teams, prohibiting surveyor conflicts of interest, and expanding CMS-based surveyor training.”
The impact:
As hospice utilization continues to climb at a rapid pace, expect increased audits and larger penalties from CMS.
What you can do:
Perform a thorough review of your hospice compliance program. Be sure to identify any potential gaps.
Address past deficiencies. Look through prior surveys and ensure you have set up processes to address any past deficiencies. A common challenge is effective, accurate, and consistent documentation.
Use a QAPI framework for assessing these areas and creating a plan for improvement. QAPI programs allow home health and hospice agencies to improve quality and performance using a systematic, data-driven approach.
The COVID-19 Vaccine Mandate
In September 2021, as part of the Path Out of the Pandemic, the Biden-Harris Administration announced that it would require COVID-19 vaccination of all staff within Medicare- and Medicaid-certified facilities.
CMS released its final interim rule on November 4, 2021, which requires full vaccination of healthcare providers and staff by January 4, 2022. Facilities must formulate a vaccine policy and ensure that employees have received their first shots by December 5, 2021. (Note that private practices are exempt from this rule, according to the American Physical Therapy Association.)
Healthcare facilities found not complying with the CMS mandate requirements by December 5, 2021, will be given a warning and a chance to comply. But CMS has stressed that it will exercise its full authority to bring organizations into compliance with the mandate.
The impact:
Because many employees are concerned about getting the vaccine, it’s possible that agencies could lose a percentage of their staff, placing an additional burden on remaining employees, lowering capacity, straining resources, and affecting morale.
What you can do:
Implement technology that allows you to do more with less. Care delivery is more efficient and effective when organizations can standardize treatment approaches based on best practices. One key strategy for improving care standardization is employing digital care pathways based on the latest evidence-based best practices, so that you can more easily scale high-quality care to your patient population and reduce unnecessary visits.
Improve your onboarding and training. Efficient, effective onboarding and training can allow you to get new hires or back office staff in the field faster with the skills they need to succeed, while improving satisfaction, engagement, and retention.
Continue to manage burnout and boost morale. Help your employees feel heard, acknowledged, and valued with strategies like empathetic listening, asking staff for suggestions on what would make their work easier from day to day, establishing a provider wellness committee, and implementing a peer-to-peer coaching program.
How MedBridge Helps
Onboarding and Training
The MedBridge Onboarding Solution allows you to get new hires in the field faster with the skills they need to succeed. With our efficient and effective solution, you can standardize and scale engaging training programs; automate enrollment, assignment, and notifications; and identify and remediate gaps in knowledge.
The MedBridge OASIS Training Solution features an onboarding series that helps frontline staff learn how to accurately gather and utilize OASIS data, as well as OASIS booster courses designed to reinforce training annually or remediate skill gaps with five- to ten-minute microlearning videos.
Patient Engagement and Management
The MedBridge Home Health Care Solution features effective patient engagement and management tools that allow you to expand clinical capacity, while reducing cost per episode, unnecessary onsite visits, and readmissions with standardized care pathways.
Quality and Performance Improvement
The MedBridge Home Health Team can help you create and implement an effective QAPI program across your agency. Along with expert consultation, we offer effective, best-in-class staff and patient education, patient engagement tools, and reporting and analytics capabilities for home health agencies looking to remediate areas of low performance, drive quality care, and improve outcomes.
The MedBridge Documentation Education Solution includes advanced course series, webinars, onboarding programs, and automated tools that allow you to distribute, scale, and standardize training on the latest, most effective documentation standards.
Communicating with Staff and Preventing Burnout
We offer a number of courses for preventing and addressing staff burnout and better communicating with your employees:
Addressing Burnout in Healthcare: course series by Erika del Pozo
Social Isolation, Occupational Disruption, and Mental Health in COVID-19 (Recorded Webinar)
Curb Your Crisis: When Drive Is in Low Gear