Remote Therapeutic Monitoring: Rate Updates and 2024 Proposed Physician Fee Schedule

Are you and your billing team up to date on all the changes to remote therapeutic monitoring (RTM)? Here’s the latest news and updates affecting RTM from a regulatory and reimbursement standpoint.
Note: Organizations with billing-specific questions should seek clarification from their payers and the APTA.
Proposed Changes in 2024
On July 13, 2023, CMS released the 2024 Proposed Physician Fee Schedule and with it several proposed updates to RTM that organizations and providers should be aware of and watch for in the final rule. If adopted, the proposed changes below would take effect January 1, 2024.
Proposed clarifications
- With the expiration of the Public Health Emergency (PHE), RTM is only available to established patients, not new patients.
- RTM and RPM can not be used together, but can be combined with Chronic Care Management (CCM), Transitional Care Management (TCM), Behavioral Health Integration (BHI), Principal Care Management (PCM), and Chronic Pain Management (CPM) services as long as time is not double counted.
- RTM services may be furnished and reimbursed separate and apart from the global services payment for surgery.
Proposed changes to billing
- Billing 98980 and 98981 will require 16 days of monitoring before being billed.
- CMS is proposing to allow rural health clinics (RHCs) and federally-qualified health centers (FQHCs) to bill HCPCS code G0511 for RPM and RTM services.
Proposed changes to supervision
- RTM-specific general supervision policy for PTs and OTs in private practice. In the proposal, PTs and OTs would be able to provide supervision to PTAs or OTAs providing RTM monitoring services that are not physically in the same building with them.
Request for comments
- CMS is requesting comments on many areas, including “the opportunities and challenges related to our coverage and payment policies.” We encourage providers and organizations to submit their comments on the rule before the deadline, September 11, 2023.
Updates to the APTA Practice Advisory for RTM
The APTA issued their last update to the advisory on March 9, 2023; however, this continues to be updated as RTM develops. We recommend that providers watch closely for updates to this key document, which provides guidance on when and how to apply each RTM code.
Medicare Administrative Contractors Won’t Issue LCD—For Now
Novitas issued the statement below, indicating that the status quo would continue for the time being in regards to reimbursement and coverage levels:
“Novitas and First Coast greatly appreciate the comments and evidence we received as a result of the multi-jurisdictional Contractor Advisory Committee (CAC) meeting that was held on February 28, 2023, regarding remote physiologic monitoring (RPM) and remote therapeutic monitoring (RTM) for non-implantable devices. After careful consideration, Novitas Solutions and First Coast Service Options will not develop a LCD for RPM and RTM for non-implantable devices. All the information and feedback received, along with any new evidence that becomes available, will be carefully considered if we decide to develop an LCD in the future.”
The recording of the CAC meeting can be viewed at the Novitas website.
Updates to the RTM rates in the Physician Fee Schedule Look-up Tool
Organizations may note that these rates have been updated since their initial posting for 2023. Facility rates for 98975 and 98977 are listed as N/A, defaulting to the non-facility rate. These and the rest of the current national rates* are displayed in the table below. Organizations receiving differing rates from those listed in the tool for their regional MACs may wish to verify reimbursement from their MAC.**
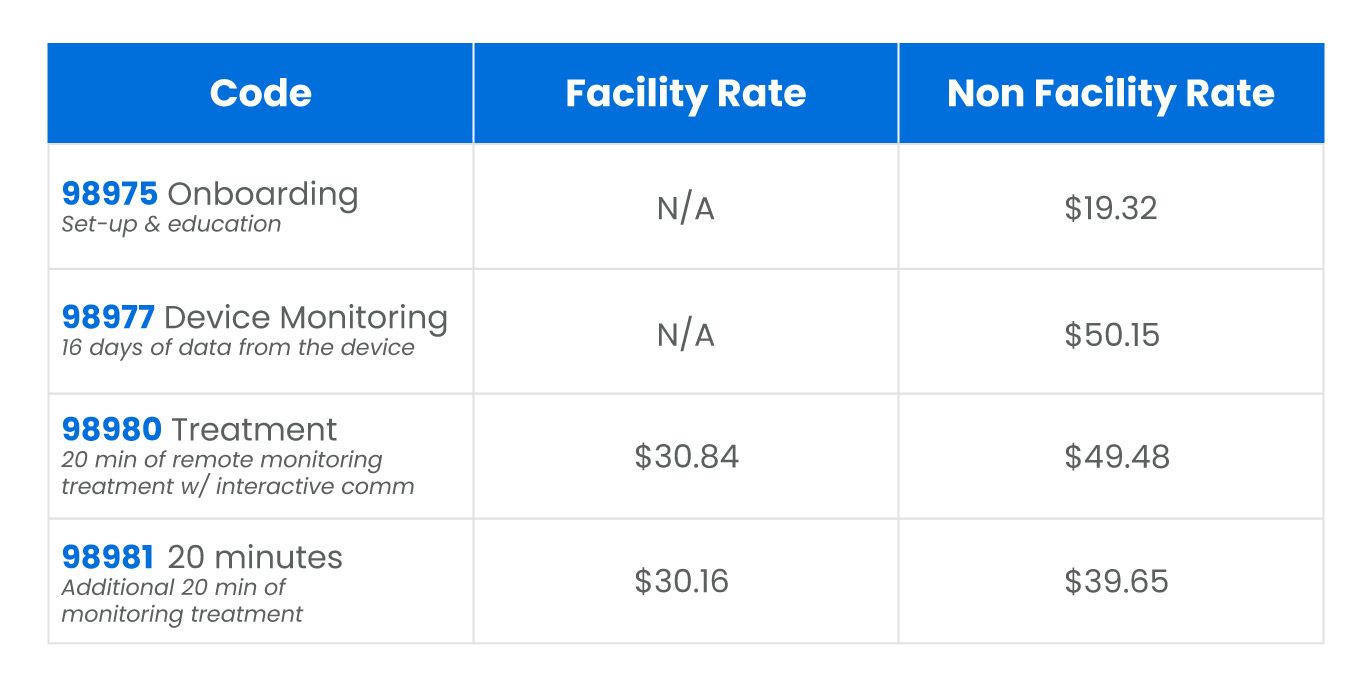
*Rates are current as of 7/5/2023
**Non-Medicare rates for remote therapeutic monitoring may vary from the rates displayed here.
If you want to learn more about MedBridge’s award-winning RTM solution, reach out to our team to set up a demo.




