What Is the Value of Subtalar Neutral for Diagnosis and Orthoses?

Subtalar neutral (STN), its importance, and its value in assessment and aligning orthoses have been argued for many years. Despite these disagreements, subtalar neutral has clinical applications and value. Better understanding the questions surrounding STN and its definition, particularly as it relates to pronation and supination, will help you determine whether to incorporate this measure into your own clinical work.
Why the Controversy?
Why are some clinicians so reluctant to assess STN?
1. Reliability
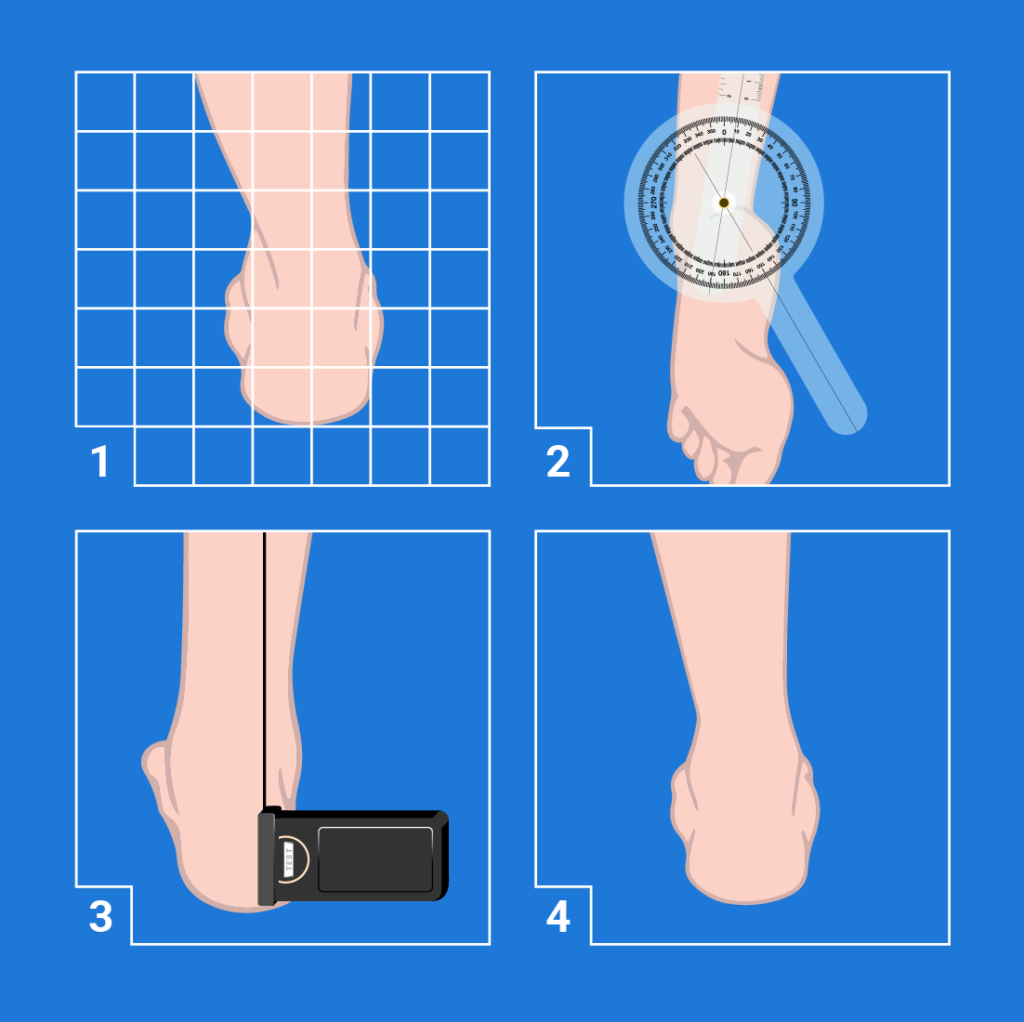
Measurement of STN has been plagued by poor reliability, and it can be difficult to trust and utilize a measure that is not repeatable. One of the factors that contributes to this problem is the drawing of the heel bisection line.
Some clinicians try to estimate the midline during their measurement or draw it free hand. Calipers have been shown to increase the reliability in unpublished data1 along with using the same heel bisection line for measurement of resting calcaneal standing position (RCSP) and neutral calcaneal standing position (NCSP).2 This ensures that, even if there is error in the bisection line drawing, the change in the heel posture from resting to neutral can be assessed and used to determine how you should prescribe posting of a foot orthosis.
The same heel bisection line used for measurement should be on the heel during the slipper casting process so it will transfer into the slipper cast to be used as a reference. You can then tell the pedorthic lab how to set the heel bisection line using posting, based on the measurements taken in standing.
Identification of STN also has error associated with it. Piernowski found that experts positioning feet in STN were within three degrees of each other as measured by a motion analysis system and this included error associated with the computerized motion analysis.3 The reliability of the navicular drop test,4 which measures navicular tubercle height in NCSP and RCSP, supports the interpretation that STN can be reliably attained with practice.
2. Importance
McPoil, et al., argue that measuring STN has no clinical relevance since we usually do not set hind foot alignment to neutral in foot orthoses but rather aim to achieve vertical heels. He also notes that avoiding end-range posture decreased symptoms in most of his patients, who are usually athletes and people with diabetes.5
Clinically, while the literature supports (and I have found) that some patients benefit from over-the-counter orthoses that stop them moving into end-range positions,6 patients who have high weight7 or high use8 benefit from having a biomechanical examination. This can identify excesses or asymmetries in foot postures with subsequent effects on lower extremity alignment and functional leg length (iliac crest height). Subtalar neutral is an important zero position for pronation and supination with respect to each person’s individual morphology.
Definitions
 Before we go further, it will be helpful to define these three important statuses we are hoping to measure: pronation, supination, and subtalar joint neutral.
Before we go further, it will be helpful to define these three important statuses we are hoping to measure: pronation, supination, and subtalar joint neutral.
Pronation is a triplanar motion of the foot in the open kinetic chain encompassing eversion, dorsiflexion, and abduction. Pronation causes the foot to move into an up and out position. When viewed in two dimensions from behind, the motion of eversion is the main posture observed.

Supination is a triplanar motion of the foot in the open kinetic chain encompassing inversion, plantar flexion, and adduction. Supination results in the foot moving into a down and in position. When viewed in two dimensions from behind, the motion of inversion is the main posture observed.

Subtalar joint neutral is an anatomical zero position of the hindfoot, clinically found through palpation of dimples around the ankle (known as palpating maximum congruence of the talo-navicular joint). It is believed to correlate to the neutral position and maximum congruency of the subtalar joint, specifically the posterior facet of the talus with posterior facet of the calcaneus. The posterior subtalar articulation is the largest size articulation of the subtalar joint.9
Zero Positions of the Hind Foot
Four different positions allow for labeling of pronation and supination (or eversion and inversion). While these are not the same position, in different contexts they are all viewed as “zero” positions.
1. In standing position or during the stance phase of gait, vertical is often considered the “zero” posture of the hindfoot. This is the American Academy of Orthopaedic Surgery’s definition.
2. For goniometric measurements, the “zero” position is in prone, when the heel bisection line is in line with the calf bisection.10
Root, et al., described these other two positions in standing:11
3. Neutral calcaneal standing position (NCSP), also known as neutral calcaneal stance position, is the posture of the heel bisection line relative to vertical while the subject is standing and guided by the examiner to attain and hold subtalar neutral position.
4. Resting calcaneal standing position (RCSP), or resting calcaneal stance position, is the posture of the heel bisection line relative to vertical while the subject is standing. Some gait studies have used the posture the subject assumes in standing as a zero point and then report pronation and supination around that “zero” point. However, most people do not naturally assume a vertical heel position nor a STN position bilaterally, so the motion reported in these studies is difficult to interpret relative to those other zero positions.
Why Do We Care?
So why does all of this matter? Why do we care about subtalar neutral, the anatomic/morphological neutral?
Measurement—Measuring the position of the heel bisection line relative to vertical while the patient is standing as they usually stand (RCSP) and then measuring the angle of the same heel bisection line when the hind foot is positioned in subtalar neutral (NCSP) allows quantification of the amount of collapse, or motion, relative to vertical. It lets us see posture relative to the patient’s individual maximal hind foot congruency. The navicular drop test and variations of this test have been shown to be more reliable than measuring the heel bisection line relative to neutral, but that test quantifies midfoot collapse rather than hindfoot collapse, and while movement between the midfoot and hindfoot is related, they are not necessarily the same.
Intervention—Using the heel bisection posture in standing and knowing this position relative to vertical and neutral are useful when posting foot or ankle foot orthoses using a neutral position slipper cast where the heel bisection line used in the examination transfers in to the cast and can be used to optimize posting. These measures are also useful when looking for symmetry or asymmetry between the feet and trying to achieve level iliac crest posture in standing. Pronation is often a mechanism the body uses to functionally shorten a longer lower extremity, and supination may be used to functionally lengthen a shorter lower extremity.
- LaPoint, S. J., Peebles, C., Nakra, A., & Hillstrom, H. (2001). The reliability of clinical and caliper-based calcaneal bisection measurements. Journal of the American Podiatric Medical Association, 91(3): 121–6.
- Spörndly-Nees, S., Dåsberg, B., Nielsen, R. O., Boesen, M. I., & Langberg, H. (2011). The navicular position test—a reliable measure of the navicular bone position during rest and loading. International Journal of Sports Physical Therapy, 6(3): 199–205.
- Sessions, J. (2019). Understanding the impact of disruptive innovation in the custom foot orthoses market. Podiatry Today, 32(2). Retrieved from https://www.podiatrytoday.com/understanding-impact-disruptive-innovation-custom-foot-orthoses-market
- Browning, R. C. & Kram, R. (2007). Effects of obesity on the biomechanics of walking at different speeds. Medicine & Science in Sports & Exercise, 39(9): 1632–41.
- Kannus, V. P. A. (1992). Evaluation of abnormal biomechanics of the root and ankle in athletes. British Journal of Sports Medicine, 26(2): 83–89.
- Deng, F. & Jones, J. (2019). Talocalcaneal joint. Radiopaedia. Retrieved from https://radiopaedia.org/articles/talocalcaneal-joint?lang=us
- Norkin, C. C. & White, D. J. (2009). Measurement of Joint Motion: A Guide to Goniometry. Philadelphia, PA: F. A. Davis Company.
- Root, M. L., Orien, W. P., Weed, J. H., & Hughes, R. J. (1971). Biomechanical Examination of the Foot Vol. 1. Los Angeles, Clinical Biomechanics Corporation.