Unbuttoning the Complex Chronic Boutonnière Deformity

What Is a Boutonnière Deformity?
A boutonnière deformity—or buttonhole deformity—involves a proximal interphalangeal (PIP) joint flexion contracture with distal interphalangeal (DIP) joint hyperextension.
This occurs due to disruption within the extensor system, specifically:
- The central slip loses the ability to extend the PIP.
- Lateral bands slide volar and become PIP flexors.
Rheumatoid arthritis can also lead to Boutonnière deformities.3
How are Boutonnière Deformities Classified for Treatment?
Boutonnière deformities can be classed as:
- Acute non-surgical
- Open acute post-surgical
- Chronic non-surgical
- Chronic post-surgical
What Is the Best Non-Surgical Way to Conservatively Treat a Chronic Boutonnière Deformity?
The boutonnière deformity can be challenging to treat conservatively, but the best ways are:
- Serial casting–Utilized in an attempt to obtain full PIP extension. During casting and over the six to eight weeks of the orthosis-weaning process, it is important for the patient to complete distal interphalangeal joint flexion exercises to promote dorsal migration of the lateral bands, delaying full motion until full active PIP extension is achieved.
- DIP joint motion–Helps to draw the lateral bands dorsal to the PIP joint axis of rotation.5
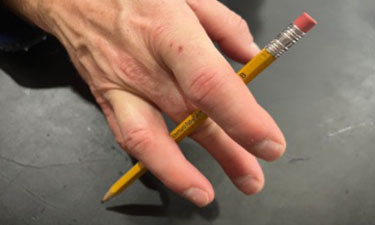
- A relative motion orthosis can also be used for patients with full PIP extension with the pencil test. This orthosis places the metacarpal phalangeal joint in 20 more degrees of flexion than the lateral digits.4,8
- Patient with a boutonnière deformity is performing the pencil test to the 3rd digit, demonstrating full PIP extension. This is a good candidate for a relative motion orthosis.
- A relative motion orthosis places the 3rd metacarpal phalangeal joint in 20 more degrees of flexion than the lateral digits promoting PIP extension.
Serial casting can be very effective in increasing PIP joint extension in chronic cases, but DIP joint active flexion must be encouraged to promote the dorsal migration of the lateral bands. A relative motion orthosis is a good option for those with full PIP extension with the pencil test. While treating chronic boutonnière deformity can be a long process, with both the therapist and the patient, good outcomes are possible.
- Cole, T., Robinson, L., Romero, L., & O’Brien, L. (2019). Effectiveness of interventions to improve therapy adherence in people with upper limb conditions: A systematic review. Journal of Hand Therapy , 32(2), 175. https://doi-org.ezproxy.gvsu.edu/10.1016/j.jht.2017.11.040
- Evans, R. B. (2012) Managing the injured tendon: current concepts, Journal of Hand Therapy , 25, 2, 173-189
- Feldon. P., Terrono, A. L., Nalebuff, E.A., Millender, L.H. (2005) Rheumatoid arthritis and other connective tissue diseases. In: D. Green, R. Hotchkiss, W. Pederson, S. Wolfe (Eds.) . Green's Operative Hand Surgery. 5th ed. (pp. 2049–136). Churchill Livingstone.
- Lalonde, D. (2015). Managing Boutonniere and swan-neck deformities. BMC Proceedings, 9 (Suppl 3)
- Lutz, K., Pipicelli, J., Grewal, R. (2015) Management of complications of extensor tendon injuries. Hand Clinics, 31(2): 301-10.
- Porter, B. J., Brittain, A. (2012) Splinting and hand exercise for three common hand deformities in rheumatoid arthritis: a clinical perspective. Current Opinion in Rheumatology, 24(2):215-21. doi: 10.1097/BOR.0b013e3283503361.
- Pratt AL, Burr N, Grobbelaar AO. A prospective review of open central slip laceration repair and rehabilitation. J Hand Surg. 2002;27(6):530e534.
- Strauch RJ. Extensor tendon injury. In: Wolfe SWW, Hotchkiss RN, Pederson WC, Kozin SH, eds. Green’s Operative Hand Surgery. 6th ed. Philadelphia, PA: Elsevier Churchill Livingstone; 2011:166e167.
- Arslan, Ö. B., Sığırtmaç, İ. C., Ayvalı, C., Baş, C. E., Ayhan, E., Bilgin, S. S., & Öksüz, Ç. (2022). The use of relative motion flexion orthoses for chronic boutonniere deformity. The Journal of Hand Surgery, S0363-5023(22), 00464-6. https://doi.org/10.1016/j.jhsa.2022.08.007