Fall Prevention Program Best Practices to Prevent Rehospitalization and Emergency Department Visits

Falls are one of the most prevalent events contributing to rehospitalizations and the leading cause of fatal and non-fatal injury in older adults. By implementing a fall prevention program, home health agencies can demonstrate their ability to deliver high-quality care, promote patient safety, and effectively manage patients’ health conditions. This positively impacts their overall quality performance scores, which, in turn, influence their reimbursement rates and reputation.
For many home health agencies, rehospitalizations and emergency department visits are ongoing challenges that cause a variety of negative impacts, from Medicare penalties to low patient satisfaction and star ratings. Under the Home Health Value-Based Purchasing (HHVBP) model, ED visits and hospitalizations are considered adverse events and indicators of potential gaps in care coordination and management.
Why Do Falls Lead to Rehospitalization?
Falls are one of the most prevalent events that contribute to rehospitalizations. According to fall risk data from the CDC:
In 2020, nearly 1 in 4 older adults (aged 65+) report falling.1
In 2021, approximately 39,000 older adults died due to a fall injury.2
There are a number of contributing factors for fall-related hospitalizations, including:
- Complications from chronic and non-chronic conditions leading to reduced balance or strength (for example, breathlessness due to COPD)
- Incomplete or missing patient education leading to misunderstandings about discharge instructions and care plans
- Impairments in activities of daily living (ADL) function
- Home layout, poor lighting, or slippery floors
- Poor patient engagement and compliance
- Inadequate transitions of care
- Medications that can lead to drowsiness or lightheadedness
- Mobility issues following surgery or from a condition like Parkinson’s disease
- Lack of physical activity leading to deconditioning/muscle weakness
But a recent report released by the U.S. Department of Health and Human Services found that “55 percent of falls identified in Medicare claims were not reported in associated OASIS assessments as required,”3 demonstrating the importance of ensuring that staff are properly trained to document accurately, because:
– 35 percent of the quality score is attributed to OASIS accuracy.
– 35 percent is based on submitted claims for emergency department visits, as well as hospitalizations that occur within the first 60 days a patient receives service.
– Over half of hospitalizations from home health occur within the first 14 to 21 days of start of care.4
You can imagine the additional cost to an agency’s reputation and bottom line in a scenario where a patient experiences a fall-related hospitalization that is then not reported accurately into the OASIS!
How to Create a Fall Prevention Program with Clinical Training and Education
Clinical Training on Fall Prevention
To effectively mitigate falls in the home, home health nurses must first understand fall risk and learn how to make adjustments to patient behavior and risk factors in the home. To prepare competent nurses for the field, you’ll need to provide skill-based training that meets national standards and requires an expert-prepared, competency-based program.
Ensure That Nurses Can Identify Fall Risk
Two of the leading contributors to increased fall risk are chronic conditions and medication adherence. Let’s see an example of how a patient not adhering to their medication schedule can increase their fall risk, and how it can be addressed.
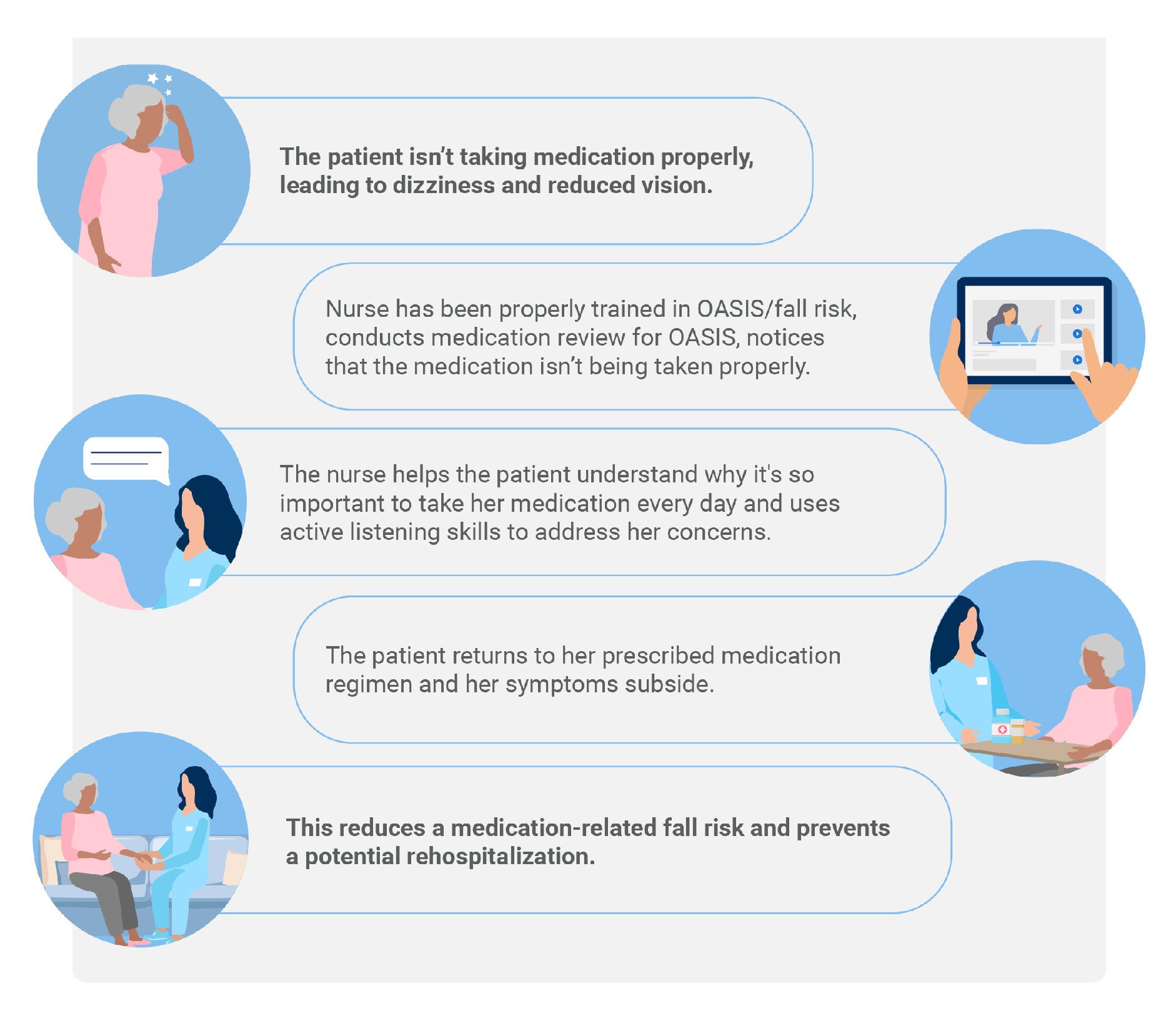
Soft Skills Training
It’s crucial that soft skills training is an important part of clinician onboarding and ongoing training, making it easier for clinicians to effectively communicate to patients so they understand the various risk factors that may be present in their home or risk factors that can be exacerbated by their health conditions.
Patient Education on Fall Prevention
The home health nurse will not be there with the patient 24 hours a day, so patients need to be adequately prepared with education on how to prevent falls, as well as what to do if a fall occurs. Educational resources and self-management tools empower patients to actively participate in improving their physical function.
A higher perception of self-efficacy after discharge from physical therapy is associated with better perceived clinical improvement, lower pain intensity, and a lower number of physical therapy sessions.5
Disengaged patients are three times as likely to have unmet medical needs and two times as likely to delay medical care.6
OASIS Documentation and Compliance Education
You need to capture the data correctly to show that the care you’re giving is working—and that’s where the OASIS comes in. The foundation for OASIS success starts with onboarding. Incorporate effective, expert-led OASIS training into your organization’s onboarding program to get your clinicians off to a good start from day one.
Addressing the PI Piece of QAPI
Patient management and quality analysis software platforms such as Homecare Homebase, Medalogix, and SHP help your agency tackle the quality analysis piece of your QAPI program by understanding which patients need more care and how well your agency is managing your patient population.
How to Create a Fall Prevention Program with MedBridge
MedBridge’s new In-Home Essentials has everything you need for point-of care clinical excellence throughout the nurse’s entire career journey, from onboarding training through mentorship and career advancement. Our home health ecosystem is designed to elevate your team by integrating:
Quality Onboarding and Fall Prevention Training
From seamless delivery of required training to digital management of the competency process, MedBridge ensures new hires are trained, skilled, and deployed in the field quickly and effectively. Our Skills and Competency Manager helps you improve quality of care and patient satisfaction, meet regulatory requirements, and reduce risk with our online skills assessment checklist and engaging, evidence-based skills training. This includes our:
Digital Skills Checklist
Prepare new hires for the field faster with a customized training program and fall prevention checklist focused on identified skill gaps.
Video-Based Nurse Skills Library
Boost knowledge retention and master home health- and hospice-specific skills with bite-sized lessons.
Reporting & Analytics Dashboard
Ensure the success of your fall prevention program by assigning checklists, simplifying preceptor assessments, and reviewing skill acquisition and sign-off data on our user-friendly dashboard.
Superior Clinical Training and Ongoing Mentorship
With MedBridge, agencies can keep employees sharp, satisfied, and supported through fast, accessible content so they can continually operate at the very top of their license, delivering outstanding care quality and helping to prevent employee turnover. Some additional resources on how to build a fall prevention program include:
[Certificate Program] Fall & Injury Prevention: How To Manage, Engage, & Evaluate
[Course Catalog] Fall Prevention Education
Five Part Fall Prevention Series featuring Dr. Pat Quigley
Use a Clinical Procedure Manual to Solidify Your Fall Prevention Program
Our tablet-ready Clinical Procedure Manual offers fast search functionality, immediately surfacing the right procedures exactly when clinicians need them. Nurses can access point-of-care training on key skills such as fall prevention, medication, and OASIS to ensure clinical excellence at the point of care. This way, nurses can walk into patients’ homes feeling confident and ready to deliver the highest standard of care, knowing that their agency and MedBridge have their back.
- Kakara R, Bergen G, Burns E, Stevens M. (2021). Nonfatal and Fatal Falls Among Adults Aged ≥65 Years. MMWR Morb Mortal Wkly Rep 2023;72:938–943. DOI: http://dx.doi.org/10.15585/mmwr.mm7235a1.
- Kakara R, Bergen G, Burns E, Stevens M. (2021). Nonfatal and Fatal Falls Among Adults Aged ≥65 Years. MMWR Morb Mortal Wkly Rep 2023;72:938–943. DOI: http://dx.doi.org/10.15585/mmwr.mm7235a1.
- US Department of Human and Health Services, Office of Inspector General. (2023) Home Health Agencies Failed To Report Over Half of Falls With Major Injury and Hospitalization Among Their Medicare Patients https://oig.hhs.gov/oei/reports/OEI-05-22-00290.asp
- Rosati, R. J. & Huang, L. (2007). Development and testing of an analytic model to identify home health care patients at risk for a hospitalization within the first 60 days of care. Home Health Care Services Quarterly, 26(4), 21–36
- Souza, C. M., Martins, J., de Càssia Libardoni, T., & de Oliviera, A. S. (2020). Self-efficacy in patients with chronic musculoskeletal conditions discharged from physical therapy service: A cross-sectional study. Musculoskeletal Care, 18(3), 365–371.
- Hibbard, J. H. & Greene, J. (2013). What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Affairs (Project Hope), 32(2), 207–14.